Fatty liver disease symptoms often stay quiet for years, even as fat slowly builds up inside liver cells and disrupts normal metabolism. This condition, now commonly referred to as metabolic dysfunction–associated steatotic liver disease (MASLD), has become one of the most common chronic liver disorders worldwide. Closely tied to obesity, insulin resistance, and type 2 diabetes, it reflects broader lifestyle shifts toward calorie-dense diets and reduced physical activity. Because early damage is reversible, understanding why fatty liver disease is increasing matters as much as recognizing who should be screened.
Many people live for years without obvious fatty liver disease symptoms, only learning about the condition after routine blood tests or imaging. By the time discomfort or fatigue appears, inflammation or scarring may already be present. This makes early awareness critical, especially for adults with metabolic risk factors.
Fatty Liver Disease Symptoms: Silent Progression and Early Warning Signs
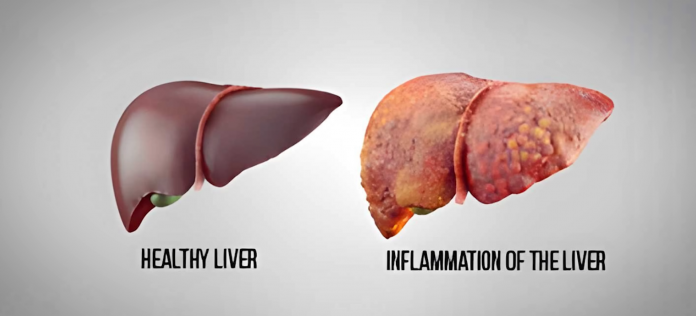
Fatty liver disease symptoms are absent in most people during early stages, which is why the condition is often found incidentally. Mild steatosis rarely causes pain, and liver enzymes may remain only slightly elevated. When symptoms do appear, they tend to reflect more advanced inflammation or fibrosis rather than simple fat accumulation.
Common fatty liver disease symptoms include persistent fatigue, vague pressure or discomfort in the right upper abdomen, and reduced exercise tolerance. As scarring progresses, more serious signs can develop, such as jaundice, abdominal swelling, leg edema, or mental confusion linked to toxin buildup. These symptoms usually indicate significant liver impairment rather than early disease.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), most people with fatty liver disease have no symptoms, and the condition is frequently discovered during testing for unrelated issues. The NIDDK also emphasizes that symptom severity does not reliably reflect how much liver damage is present, which is why imaging and lab tests are essential for proper assessment.
NAFLD Causes: Why Fatty Liver Disease Is Increasing Globally
NAFLD causes are rooted in metabolic imbalance, where excess calories overwhelm the liver’s ability to process and export fat. Insulin resistance plays a central role, driving increased fat delivery to the liver and stimulating new fat production within liver cells. Over time, this leads to triglyceride accumulation and oxidative stress.
Several forces explain the sharp global rise in NAFLD causes. Obesity rates have climbed steadily, particularly central or visceral obesity, which directly exposes the liver to free fatty acids. Diets high in refined carbohydrates and fructose-sweetened beverages accelerate liver fat synthesis. Physical inactivity further worsens insulin resistance, while disrupted sleep and chronic stress add to metabolic strain.
Based on a study conducted by the World Health Organization (WHO), the worldwide increase in obesity and type 2 diabetes closely parallels the rising prevalence of fatty liver disease, especially in urbanizing regions. The WHO highlights that lifestyle-driven metabolic disorders now represent a leading contributor to chronic liver disease globally.
Fatty Liver Disease Diagnosis: Tests, Imaging, and Risk Assessment
Fatty liver disease diagnosis usually begins with blood tests showing mildly elevated ALT or AST levels, though normal enzymes do not exclude disease. Imaging plays a key role, with ultrasound commonly identifying a “bright” liver appearance consistent with steatosis. More advanced tools help assess scarring without invasive procedures.
Transient elastography (FibroScan) measures liver stiffness and estimates fibrosis risk, while MRI-based techniques quantify liver fat more precisely. Noninvasive scoring systems such as FIB-4 combine age, liver enzymes, and platelet counts to identify patients who need specialist referral. Liver biopsy is reserved for cases where diagnosis or staging remains unclear.
According to the American Liver Foundation, noninvasive tests now allow clinicians to identify patients at risk for advanced fibrosis without routine biopsy. The foundation notes that early diagnosis enables lifestyle changes that can halt or reverse fatty liver disease before permanent damage occurs.
NAFLD Treatment: Reversal, Management, and Prevention Strategies
NAFLD treatment focuses on addressing the metabolic drivers behind liver fat accumulation. Sustained weight loss of 7–10% has been shown to significantly reduce liver fat and inflammation. Dietary patterns emphasizing whole foods, fiber, and unsaturated fats support insulin sensitivity and reduce hepatic stress.
Regular physical activity improves liver health even without dramatic weight loss, as exercise lowers visceral fat and improves glucose control. Emerging medications such as GLP-1 receptor agonists show promise in reducing steatosis and inflammation, particularly in patients with diabetes. For individuals with severe obesity, bariatric surgery can lead to substantial improvement or resolution of fatty liver disease.
Prevention remains central. Limiting sugary beverages, maintaining a healthy waist circumference, managing blood sugar, and monitoring cholesterol levels all reduce long-term risk. Early intervention offers the best chance to avoid progression to cirrhosis or liver cancer.
Fatty Liver Disease and Metabolic Health: Why Early Action Matters
Fatty liver disease reflects broader metabolic strain rather than an isolated liver problem. When liver fat builds up, it worsens insulin resistance, increases cardiovascular risk, and raises the likelihood of future diabetes complications. Addressing fatty liver disease therefore supports whole-body health, not just liver function.
Early screening in people with obesity, diabetes, or metabolic syndrome allows clinicians to identify reversible stages. Small, consistent lifestyle changes often yield meaningful improvements within months. As global rates continue to rise, recognizing fatty liver disease as a metabolic warning sign rather than a silent incidental finding can shift outcomes toward prevention and long-term health.
Frequently Asked Questions
1. Is fatty liver disease always serious?
Fatty liver disease is often mild in its early stages and may never progress in some people. However, a significant portion develop inflammation and scarring over time. The challenge is that symptoms do not reliably signal progression. Regular monitoring helps identify who needs closer care.
2. Can fatty liver disease be reversed naturally?
Yes, early fatty liver disease can often be reversed with sustained weight loss, dietary changes, and regular exercise. Even modest improvements in lifestyle can reduce liver fat. Consistency matters more than rapid results. Medical guidance helps tailor changes safely.
3. Do you need alcohol to get fatty liver disease?
No, nonalcoholic fatty liver disease occurs in people who drink little or no alcohol. It is primarily linked to metabolic factors like obesity and insulin resistance. Alcohol-related liver disease is a separate condition. Both can cause similar liver damage.
4. Who should be screened for fatty liver disease?
People with obesity, type 2 diabetes, metabolic syndrome, or persistently abnormal liver enzymes should be evaluated. Family history and certain ethnic backgrounds may also increase risk. Screening usually starts with blood tests and imaging. Early detection allows timely prevention strategies.