Why are doctors killing or stroking out thousands of people a year for nothing? How do doctors even convince patients to sign up for procedures that are all risk without benefit?
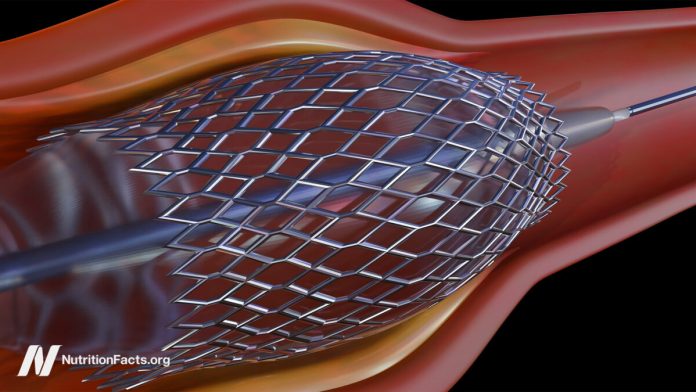
Millions of people have gotten stents for stable coronary artery disease (CAD), yet we now know that angioplasty and stent placement don’t actually prevent heart attacks, offer long-term angina pain relief, or improve survival for such patients. Why? Because the most dangerous plaques—the ones “most vulnerable to rupture or erosion—leading to a subsequent cardiac event,” that is, a heart attack, are not the ones doctors put stents into. They aren’t even the ones that are often seen on angiograms to be obstructing blood flow. So, “we need to avoid the ‘therapeutic illusion’ that we are accomplishing more than is shown by the evidence.” Percutaneous coronary intervention (PCI) looks great. Angioplasty and stents open up blood flow again, but if PCI doesn’t actually help, why do it?
We aren’t just talking about billions of dollars wasted either. Stent placement and the blood-thinner drugs that need to be taken can cause complications, including heart failure, stroke, and death, but the risks are relatively low. There is less than a 1 percent chance PCI will kill you or stroke you out, and the 15 percent risk of heart attack is only if your stent clogs off at a later date, which only happens in about 1 percent in the near term. There is a 13 percent chance of kidney injury, though, due to the dyes that have to be injected, but that typically heals on its own. The most serious complications, like death, happen in only about 1 in 150 cases, but that must be multiplied by the hundreds of thousands of procedures being done every year.
In an emergency setting, like while you’re actively having a heart attack, angioplasty can be lifesaving, but these hundreds of thousands of procedures are done for stable coronary artery disease, for which there appear to be no benefits. So, doctors are killing or stroking out thousands of people a year for nothing. And that’s not even counting the tens of thousands of silent mini-strokes that may contribute to cognitive decline caused by these procedures. Between 11 and 17 percent of people who go through angioplasty or stenting come away with new brain lesions, as you can see below and at 2:16 in my video The Risks of Heart Stents. That’s up to about one in six individuals.
How do doctors convince patients to sign up for PCI when it doesn’t lower the risks of death or heart attack, nor does it offer long-term symptom relief? Apparently, by conveniently failing to “inform the patient that PCI would not lower their risk of death or MI [myocardial infarction or heart attack], or that the symptom benefit is gone after 5 years,” thereby not offering long-term symptom relief.
Cardiologists are aware of how little they help, but studies have “consistently demonstrated” that patients think stents will reduce their risk of heart attack or death. More than 70 percent of patients erroneously believed that stents would extend their life expectancy or prevent future heart attacks. That’s why this study was done—to figure out “why patients overestimate these benefits.” Where are they getting these wild ideas? The answer is that many patients are being kept in the dark. Doctors, who overstate the benefits and understate the risks, may pressure patients into procedures that won’t benefit them the way they think. Why? Well, one reason may be because doctors may be paid per procedure. “Current reimbursement favors procedures over medication and lifestyle change, and it is possible that reimbursement may influence physicians’ recommendations.” Doctors are paid more for offering stents than recommending common sense diet and lifestyle changes.
Patients with stable coronary disease who undergo angioplasty and stent placement are frequently misinformed of the benefits. Of 59 recorded conversations between cardiologists and their patients, only two discussions included all seven elements of informed decision-making—telling people they have a choice, explaining the problem, discussing alternatives and the pros and cons, informing patients the procedure may not work, asking if they understand, asking if they have any questions, and asking them what they want to do. Only 3 percent of doctor-patient discussions about stents hit even just these basic elements! And this was the case when “the physicians and patients knew that they were being recorded, which could have affected their behavior. If so, it is likely that this represents a best-case scenario for these physicians.” Only 3 percent! Quoting from the Cleveland Clinic Journal of Medicine, when it comes to angioplasty and stents, “true informed consent rarely occurs.”
It’s no wonder that among the nearly 1,000 patients surveyed across ten U.S. academic and community hospitals, just 1 percent knew the truth. Remarkably, some blame the patients for their ignorance, saying patients are the ones who “commonly overestimate or misunderstand the benefits of treatment, such as patients with cancer who believe that palliative chemotherapy offers the potential for cure—the ‘therapeutic misconception.’”
“Why are so many patients having procedures with benefits that they poorly understand? Don’t look at the patients to find out why. Instead, examine the doctor’s motivation…Patients think they are having life-saving procedures because medical professionals want them to believe that this is so.” Now, it’s not like those 95 percent of cardiologists are lying to their patients and saying it will reduce their risk; they just happen to conveniently omit those details. But “[i]n the absence of information to the contrary, most patients and some doctors assume that PCI is life-saving and are biased towards choosing it. As a result, patients are rarely able to give true informed consent to undergo PCI.”
Why would they assume that? Because many have a wild concept of “‘personal care’—that a physician’s first obligation is solely to the patient’s well-being,” but isn’t that naïve? “In the absence of information, or even when presented with evidence to the contrary, patients tend to believe that treatments offered will be beneficial.”
It’s true, even if you explicitly tell patients that stents do not reduce the risk of heart attacks. You can cut that misperception in half “with relatively little effort—as little as 2 lines of text,” dispelling the myth in many people. But many participants continued to believe that angioplasty and stents prevent heart attacks, even when explicitly told they do not and given a detailed explanation of why they do not. After all, why would doctors be pushing them if they didn’t help? That’s a good question, which we’ll address next.